- Heartful Digest
- Posts
- The Parent's Strategic Guide to Extracting Actual Nutrition Help From Your Pediatrician (Without Getting a $500 Bill)
The Parent's Strategic Guide to Extracting Actual Nutrition Help From Your Pediatrician (Without Getting a $500 Bill)
Why most parents leave pediatric visits with generic advice about vegetables, and the systematic approach to getting personalized nutrition guidance that your insurance will actually cover
Welcome to the Heartful Sprout newsletter! Your go-to source for expert-vetted, AI-curated insights on child nutrition, development, and parenting. We’re here to answer all your questions, provide end-to-end solutions, and connect you with a supportive community of parents. www.heartfulsprout.com
From managing picky eaters to understanding developmental milestones, our mission is to empower you with the tools and knowledge to help your child thrive. Together, let’s build a healthier, happier future—one step at a time.
Picture this: You've waited three weeks for your child's appointment, sat in a waiting room that looks like a daycare center designed by someone who actively dislikes children, and finally get your precious twelve minutes with the pediatrician. You mention that little Emma subsists entirely on goldfish crackers and the occasional apple slice. The doctor nods knowingly, hands you a photocopied handout about the food pyramid (circa 1995), and cheerfully suggests "making meals fun."
Congratulations. You've just experienced the standard American approach to pediatric nutrition counseling.
The Problem: Healthcare's Nutrition Theater
Here's what the pediatric nutrition industrial complex doesn't want you to know: according to research from Colorado School of Medicine, the average pediatrician spends exactly 120 seconds discussing nutrition during a patient visit. That's barely enough time to open the EHR system, let alone develop a meaningful strategy for convincing your toddler that broccoli isn't actually a form of green poison.
Meanwhile, childhood obesity rates have tripled since 1980. Food allergies are skyrocketing. And parents are drowning in contradictory nutritional advice from Instagram influencers who apparently believe that spiralizing vegetables can solve generational eating disorders.
The typical pediatric visit goes like this: weight check, height measurement, a few questions about sleep and development, shots if needed, and then—if you're lucky—a rushed conversation about whether your child is eating "enough vegetables." The doctor types furiously into a computer that seems designed by people who've never actually practiced medicine, and you leave with a vague sense that you should probably be doing something different but zero actionable guidance.
The Typical Flawed Approaches (Prepare for Gentle Mockery)
Most healthcare technology companies have approached this problem with their characteristic combination of venture capital enthusiasm and complete disconnection from clinical reality. They've built:
The Overwhelm-o-Matic App: Platforms that require parents to log every grape, photograph every meal, and track seventeen different micronutrients while somehow maintaining their sanity and employment.
The One-Size-Fits-Nobody Solution: Cookie-cutter meal plans that ignore cultural preferences, family schedules, and the basic reality that some children would rather starve than eat green vegetables.
The AI Magic 8-Ball: Systems that promise to solve nutrition through machine learning but can't figure out that a two-year-old throwing broccoli at the wall doesn't need more complex algorithms—they need different broccoli strategies.
The Refreshingly Different Approach: Technology That Serves Humans
What if we stopped trying to revolutionize healthcare and started trying to make it work better? What if we built tools that respect both clinicians' time constraints and parents' actual lives?
This is where custom GPT solutions like HeartfulSprout enter the conversation—not as another overhyped AI miracle, but as a practical bridge between what parents need to know and what pediatricians have time to explain.
Heartful Sprout is on a mission to transform pediatric nutrition by supporting families and clinicians with smarter tools and personalized solutions. Starting January, the team is launching a pilot with leading clinicians while raising $750K to enhance their platform and scale their impact. With 24,000+ engaged parents, strong community partnerships, and innovative technology, Heartful Sprout is building a healthier future for children from the very start.
The Practical Revelation: How to Actually Get Help
Step 1: Master the Art of Strategic Pediatric Communication
Your pediatrician isn't avoiding nutrition conversations because they enjoy watching children develop preventable conditions. They're trying to document chief complaints, perform exams, order tests, code visits, respond to messages, and somehow maintain their clinical license while the EHR times out every fourteen minutes.
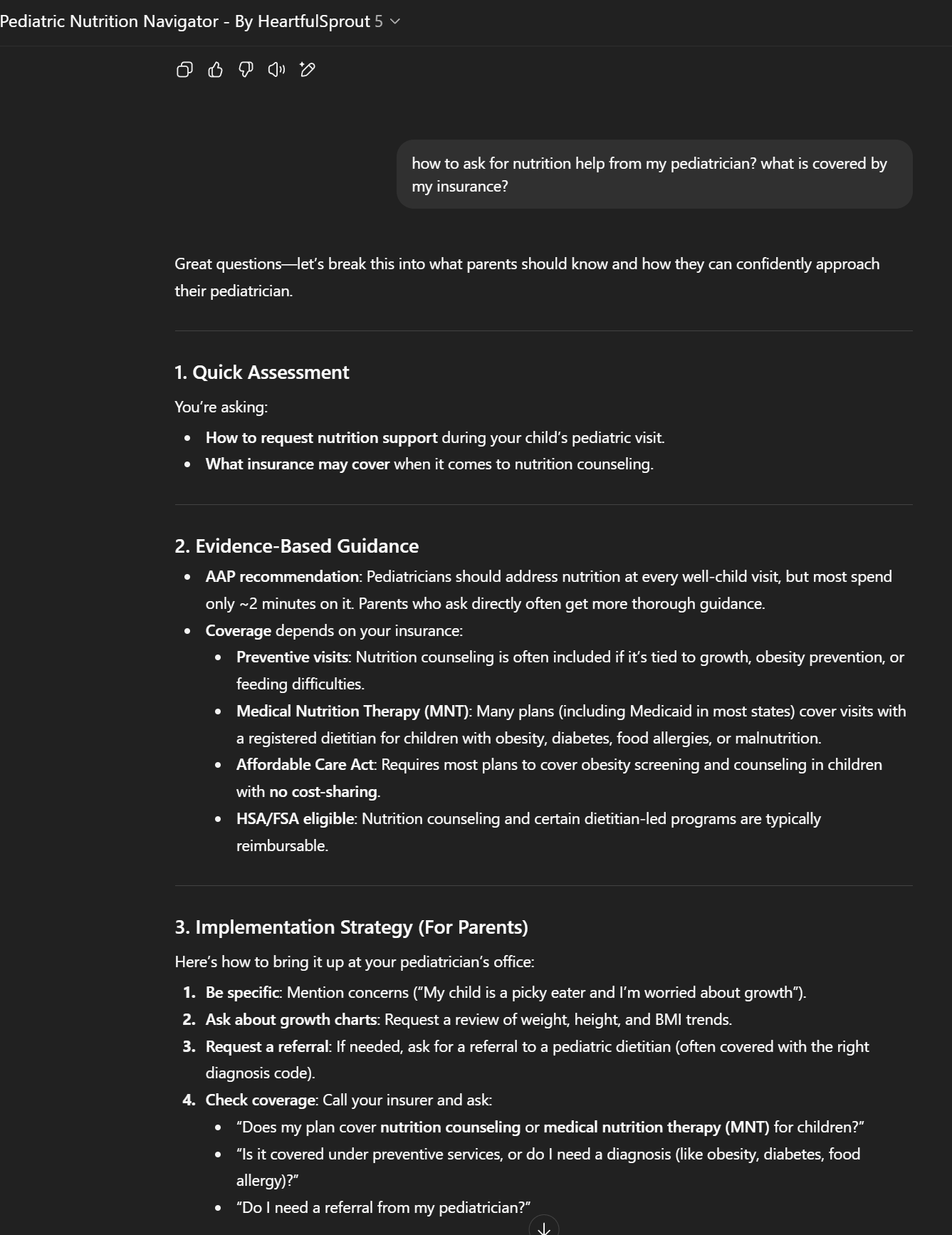
The Magic Words That Work: "I'd like to spend some time today discussing my child's nutrition and growth patterns. Can you review their growth chart trends with me and identify any areas of concern? If there are issues, I'd appreciate guidance on next steps, including whether a referral to a pediatric dietitian would be beneficial."
This approach accomplishes several things: it acknowledges nutrition as a medical concern (not just parental anxiety), requests specific data review (which pediatricians love), and opens the door for referrals (which insurance companies understand).
What Not to Say: "I read online that my child needs more superfoods" or "Pinterest says I should eliminate gluten." These phrases trigger the same physiological response in pediatricians that fire alarms cause in normal humans.
Step 2: Decode the Insurance Coverage Mystery
Here's what insurance companies don't advertise but will pay for when properly requested:
Preventive Nutrition Counseling: The Affordable Care Act requires most plans to cover obesity screening and counseling for children with no cost-sharing. This includes basic nutrition guidance during well-child visits.
Medical Nutrition Therapy (MNT): Many insurance plans, including most state Medicaid programs, cover visits with registered dietitians for children with specific diagnoses: obesity (BMI ≥95th percentile), diabetes, food allergies, malnutrition, or feeding difficulties.
The Documentation Dance: For insurance to pay, your pediatrician needs to use specific codes. The magic combinations include ICD-10 codes like Z71.3 (dietary counseling), E66.9 (obesity), or R63.3 (feeding difficulties), paired with CPT codes for preventive counseling (99401-99404) or medical nutrition therapy (97802-97804).
The Parent's Insurance Investigation Script: Call your insurance company and ask: "Does my plan cover pediatric nutrition counseling or medical nutrition therapy? Is it covered under preventive services, or do I need a specific diagnosis? Do I need a referral from my pediatrician?"
Most customer service representatives will need to transfer you twice and consult their supervisor, but persistence pays off. Document everything, including representative names and reference numbers.
Step 3: Leverage Technology That Actually Helps
This is where custom GPT solutions become genuinely useful rather than just impressive tech demos. A well-designed nutrition AI can serve as an intelligent intermediary between your concerns and your pediatrician's limited time.
Before Your Appointment: Use a nutrition-focused GPT to organize your questions, document your child's eating patterns, and identify specific concerns. Instead of saying "my child is a picky eater," you can provide data: "My child consistently refuses vegetables, eats from only three food groups, and has dropped from the 50th to 25th percentile for weight over six months."
During Your Appointment: A good GPT can generate culturally-relevant meal plans that your pediatrician can review and modify rather than creating from scratch. This transforms a potentially lengthy counseling session into an efficient review and customization process.
After Your Appointment: The same system can track implementation, monitor outcomes, and identify when follow-up is needed. This creates the kind of data continuity that makes pediatricians professionally happy and insurance companies financially cooperative.
When your pediatrician agrees that additional nutrition support would be beneficial, the referral process becomes crucial. Most pediatric practices work with specific registered dietitians who understand both insurance requirements and practical family dynamics.
The Referral Request: "Based on our discussion, would you recommend a referral to a pediatric dietitian? If so, could you provide a referral with appropriate diagnostic codes to ensure insurance coverage?"
Timing Matters: Many insurance plans require referrals to be recent (within 30-90 days) and specific to the issue being addressed. A general "nutrition consultation" referral is less likely to be covered than one for "nutrition therapy for pediatric obesity" or "dietary management of food allergies."
The Implementation Framework: Your Action Plan
Phase 1: Preparation (Technology First)
Before your next pediatric visit, invest fifteen minutes in strategic preparation. Use a nutrition-focused GPT to document your child's current eating patterns, growth concerns, and specific questions. This isn't helicopter parenting—it's efficient healthcare consumption.
Create a simple timeline: when did eating issues start, what interventions have you tried, and what outcomes have you observed? This level of organization transforms you from "anxious parent" to "collaborative care partner" in your pediatrician's mind.
Phase 2: The Appointment (Process Optimization)
Arrive with specific questions and documented concerns. Request growth chart review early in the visit. If concerns exist, ask about referral options before the appointment concludes.
Remember that pediatricians are more likely to provide thorough nutrition guidance when they see evidence of parental engagement and follow-through capability. Bringing organized questions demonstrates both.
Contact your insurance company with specific questions about coverage. Document everything. If initial responses are unsatisfactory, request supervisor review.
Many insurance companies have separate customer service lines for "benefits verification" that provide more detailed coverage information than general customer service.
Phase 4: Follow-Through (Money and Metrics)
Track the financial and health outcomes of your nutrition interventions. Document changes in eating patterns, growth metrics, and any reduced need for additional medical visits.
This data becomes valuable for future insurance negotiations and demonstrates to your pediatrician that nutrition counseling produces measurable results in your family.
Common Pitfalls to Avoid
The Information Overload Trap: Don't arrive at appointments with printouts from seventeen nutrition websites. Pediatricians respond better to specific, organized questions than to research dumps.
The DIY Diagnosis Error: Avoid self-diagnosing nutritional conditions based on internet research. Instead, present symptoms and let your pediatrician determine appropriate diagnostic considerations.
The Insurance Assumption Mistake: Never assume that insurance won't cover nutrition services. Many parents miss covered benefits because they don't ask the right questions.
The Technology Replacement Fallacy: Remember that AI tools are meant to enhance, not replace, professional medical advice. Use technology to organize information and generate options, but always review recommendations with qualified healthcare providers.
The Bottom Line: Practical Revolution
We're not promising to disrupt healthcare or revolutionize pediatric medicine. We're just making it possible for you to get meaningful nutrition guidance without requiring your pediatrician to become a miracle worker or your insurance company to develop human empathy.
The future of pediatric nutrition isn't about replacing clinical judgment with artificial intelligence. It's about using intelligent tools to make good healthcare more efficient and accessible.
Your next step? Schedule your child's next well-visit and come prepared with specific questions about nutrition and growth. Use technology to organize your thoughts, but trust human expertise to guide your decisions.
Because at the end of the day, the best nutrition plan is the one your family will actually follow, your pediatrician can support, and your insurance will cover.
Ready to try a smarter approach to pediatric nutrition? HeartfulSprout's custom GPT can help you prepare for productive conversations with your pediatrician and navigate the insurance coverage maze. It won't replace professional medical advice, but it will help you ask better questions and get better answers.
Access the tool here: HeartfulSprout Custom GPT - A practical nutrition planning assistant designed for real families dealing with real pediatric eating challenges.
….